Comforting a whole person: does it matter if we miss a part?

Written by Johanna Lynch – University of Queensland
A few years ago – a mentor encouraged me to read a fantastic little book by John Allen called Restoring mentalising in attachment relationships: Treating trauma with plain old therapy. There was a question in this book from mentalising expert Peter Fonaghy that has stuck with me, haunted me, and inspired some of my research and writing. It is even in the first paragraph of my book on whole person care1:
What happens to states of mind, when terror or grief is not met by reasonably attuned comforting?2p.xiii
As a General Practitioner, I have also added questions to this: What happens to… bodily states, behaviours, hearts, relationships, and communities… when they are not met by reasonably attuned comforting? Within this question is a deeper question – what is ‘reasonably attuned comforting?’
People are complex and layered. Sometimes we are only shown a small part of a person while they work out whether to trust us. Often there are other hidden parts of the person that they feel are ‘unpresentable’ or hold a risk if exposed. Sometimes the person has very reasonable fear associated with terrifying or overwhelming memories that they have pushed to the side and instinctively know they are not yet ready to touch. Other times they need encouragement to face something and discover they are now able to encounter their childhood distress with adult resources. Sometimes, we are only invited to care for a part of a person at first, and over time, inside a reliable and consistent relationship more layers of the person appear.
So – what is attuned comforting? This question is at the heart of all relationships. It is an essential part of relationships between an infant and their carer, between friends, and lovers, or even between colleagues and leaders in safe working and learning environments. It is a sophisticated dyadic and embodied kind of attention that paces connection, regulates experience, and builds sense of safety across the whole person.
The Oxford English Dictionary describes the word attuned as a verb and an adjective that means ‘to bring into harmony or accord’. In practice, tuning in to one another requires sophisticated sensing and responding between people. Daniel Seigel describes a “mutually resonant form of interpersonal communication” or aligned “states of mind” that contribute to safe attachment.3 This complex task requires careful observation and sending words and tone of voice or touch as probes into the space between people, and then sensing that response in a moment by moment way. It can include sensing that someone only wants to reveal a part of themselves and aligning with that. At other times it can involve tuning in to see hidden parts of a person and responding with signals that they are seen, welcome and included too. Sometimes, especially in a therapeutic or close relationships it may involve intentionally reaching out towards parts of a person that feel unlovable or threatened. It can be a way of ‘being with’ that sometimes has no words, with subtle changes in our posture, tone of voice, and movements. It does require that we are aware of the many layers of the whole person.
And who decides if something is comforting? How do we know that our attempts to care have been helpful? These are deep and important questions for anyone who seeks to be a healer in their community.
The Merriam-Webster dictionary defines comfort as: ‘to give strength and hope to (to cheer); and ‘to ease the grief or trouble of’ (to console). That word ‘console’ is defined by the Oxford Dictionary as ‘to alleviate the sorrow of a person, to free from the sense of misery’. This mixture of easing, alleviating and relieving AND giving freedom, strength, and hope are at the heart of comforting. Comforting is not just being made comfortable. It is not the same as withdrawing from life or avoiding tension or struggle. Strangely, bringing comfort is almost the opposite of avoidance: it involves bravely going towards pain and sorrow, for the sake of facing and knowing and growing. It is also paced in a way that facilitates calm – using humour, distraction, music, and even silence to communicate safe care of the whole person. It is a proactive building of sense of safety that enables growth.
When we teach parenting using the Circle of Security Model there are two aspects of normal development – running home to welcoming arms, that help us organise and understand our experience AND being delighted in while stepping outwards to explore the world. Courage to explore and engage with life is the natural result of attuned comforting. Those who study grief report a natural oscillation between attending to what we have lost and keeping on living.4 This flow of connection between loss and restoration can only occur if someone is safe enough to grieve.1 Attuned comforting sees and hears and walks alongside (and even mourns with us sometimes) as we face life and grow in confidence to be our real selves in the world. This is being safe enough to grow.
My doctoral work explored a strengths-based and healing-oriented approach to trauma-informed whole person care: Sense of Safety. Sense of Safety is a whole person experience that is a foundation for normal physiology, social and neurodevelopment, learning, existential ease, and bodily calm. The Sense of Safety approach is a way to deliver care and a goal of care. In this framework, Sense of Safety builds both a sense of comfort and of courage.

| Figure 1: Reprinted with permission from Lynch, J.M. (2021) A whole person approach to wellbeing: building sense of safety. Routledge. London. |
The goal of building Sense of Safety aligns with the stages of trauma-informed care first described by Judith Herman5 as ‘establishing safety, remembrance and mourning, and reconnecting with ordinary life’. This was later described in Blueknot Foundation’s guidelines6 as ‘stabilisation, processing, and integration’. The Sense of Safety Approach names these steps as: ‘building sense of safety, safe enough to grieve reality, and safe enough to grow’.1
So – back to the opening question – when we are trying to comfort a person, does it matter if we miss a part?
Knowing how wide and deep to look and sensing how welcome our attempts to reach out are, is part of the art of healing. It is also a practical question. One physician, Robert Centor suggests that we… must ‘understand the whole story… gather the history at appropriate depth’.7p.59 What is appropriate depth?
In my doctoral work on Sense of Safety I came to realise that whole person care requires at the very least, an awareness of the various ways that humans can be threatened and can sense safety. There are many ways that sense of safety can be built and lost.
My doctoral research asked the questions ‘what causes threat?’ and ‘how do you sense that you are safe?’ to participants (people with a lived experience of mental illness, First Nations academics, rural and urban GPs, and multidisciplinary mental health clinicians).1,8 Analysis initially looked at the content – what people described – and themes emerged that are called the Sense of Safety Whole Person Domains. These domains are a kind of map or overview that define the breadth of layers that might be affecting how safe someone feels:
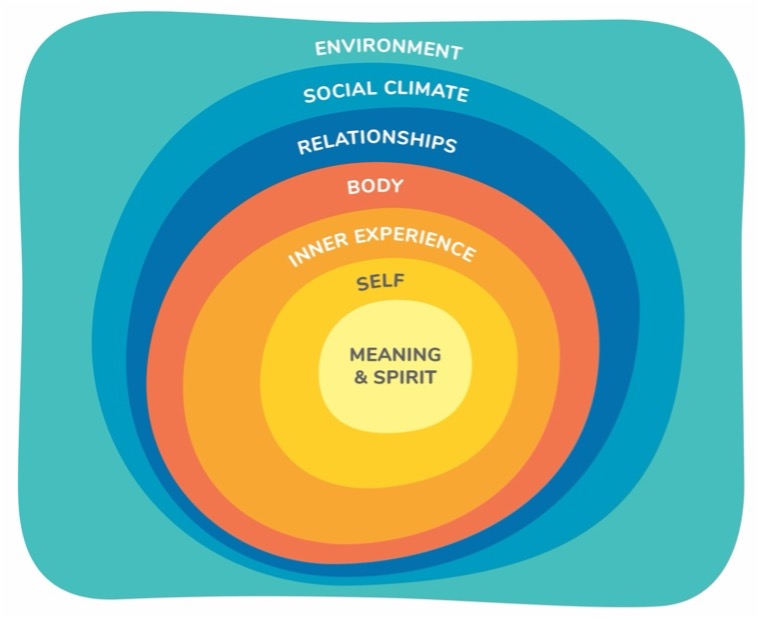
| Figure 2: Reprinted with permission from Lynch, J.M. (2021) A whole person approach to wellbeing: building sense of safety. Routledge. London. |
Environment: including the presence or absence of justice, housing, finances, policing and political security, and food and water security.
Social climate: experiences of respectful and hope-filled community relationships and stories, in places where people live, work, and learn (or of bullying, aggression, addiction, hopelessness, frightening community stories, poverty, and witnessing harm to others).
Relationships: presence of respectful connections in personal relationships – who is there, who is missing, and are they available, tuned in, and on your side?
Body: experiences of calm, rest, and regulation of emotion, or of overwhelming embodied emotion, pain, insomnia, or illness.
Inner Experience: settled, ordered, and unified (or chaotic, rigid, or fragmented) internal thoughts, visions, perceptions, attention and dreams or nightmares.
Sense of Self: A settled sense of relationship with self – connected and internally compassionate, or experiences of self-stigma, internal ignoring, hatred or betrayal.
Spirit/Meaning: existential sense of meaning and knowing place in the world, or beliefs or experiences of existential unease, ostracism, shame or guilt.
Each of these Whole Person Domains are outlined in the image above – as a kind of map to guide clinicians to notice the breadth and depth of ways that a person can be sensing safety or harm. Being aware of both sense of safety and threat can make us tune in to the reality of where the person is at. These layers of the person can guide us to notice the whole, including hidden, shameful parts as well as gifts and strengths even the person themselves might not be aware of. Even though there are times we have to wait for the person to feel able to show us all parts of them, it is really important that we stay aware of the whole person. These seven domains of a whole person can help us to stay aware of any parts that have not yet been revealed. We can then actively wait for them to become part of healing care.
Unfortunately, some scientific approaches to distress have not remained aware of what they are leaving out of their assessment of the person. Although social determinants of health are the key drivers of mental distress – they are often ignored in psychiatric frameworks of mental illness.9 Similarly, culture, spirituality, and sense of self are often not included in psychiatric or mental health formulations.10,11 Relationships and life story are also often left out of mental health assessments. A key neurobiologist has called into question many psychiatric diagnoses that have not included any information on the participants’ experiences of childhood adversity – he says these diagnoses need to be “re-evaluated to take into account the possible prepotent confounding influence of maltreatment”.12p.664 Some studies of behaviour do not attend to the rest of the body, or to the inner experiences that are part of that behaviour. As behavioural approaches to assessment have increased, awareness of inner experience or consciousness has become a less valued part of care13 – this has had far reaching impacts on conceptualisations of mental health and adequate healthcare. Diagnoses that claim certainty but take an interest in only a part of a person offer spurious precision. Not seeing a whole person causes harm – a kind of ignoring of their inner and outer connections. We should therefore critique research, diagnoses, or treatment that only cares for a part of a person without care for the whole.
Abraham Maslow reminded that threat impacts “a whole human being … never a part of a human being’.14p.75 He also noted that overwhelming experiences cause people to ‘disintegrate’.14p.11 If one part of a person hurts, the whole hurts – so if we miss something, it matters.
Balfour Mount and colleagues who wrote on suffering and wholeness remind: ‘Suffering occurs with perceived threat of destruction and ends when the threat has passed or a sense of integrity is otherwise restored’.15p.372 This confirms the underlying research into threat that underpins the Whole Person Domains.
Tuning in to the whole and restoring someone to wholeness is the central task of healing. Creating a place that is safe for all parts or layers of the person to be seen is the particular gift of a healer. Let’s ask a new question: what happens when terror or grief is met by reasonably attuned comforting? Peace, inner kindness, steady sense of self, capacity to regulate emotion, respectful connected relationships, and communities filled with spaces for belonging. Let’s all offer the healing art of seeing and caring for the whole person!
The author would like to thank Rubayyat Hashmi for their review of an earlier draft.
- Lynch JM. A Whole Person Approach to Wellbeing: Building Sense of Safety. Routledge; 2021
- Allen JG. Restoring mentalizing in attachment relationships: Treating trauma with plain old therapy. American Psychiatric Publishing; 2013.
- Siegel DJ. Toward an interpersonal neurobiology of the developing mind: Attachment relationships,“mindsight,” and neural integration. Infant Mental Health Journal. 2001;22(1-2):67-94.
- Stroebe M, Schut H. The dual process model of coping with bereavement: A decade on. OMEGA-Journal of Death and Dying. 2010;61(4):273-289.
- Herman JL. Trauma and recovery: The aftermath of violence–from domestic abuse to political terror. Hachette UK; 2015.
- Kezelman C, Stavropoulos P. Practice Guidelines for Treatment of Complex Trauma. Blue Knot Foundation 2019.
- Centor RM. To be a great physician, you must understand the whole story. Medscape General Medicine. 2007;9(1):59.
- Lynch JM. Sense of Safety: a whole person approach to distress. University of Queensland; 2019.
- Shim R, Koplan C, Langheim FJ, Manseau MW, Powers RA, Compton MT. The social determinants of mental health: An overview and call to action. Psychiatric annals. 2014;44(1):22-26.
- Fabrega Jr H. Culture, spirituality and psychiatry. Current Opinion in Psychiatry. 2000;13(6):525-530.
- Dowrick C. Person-centred Primary Care: Searching for the Self. Routledge; 2017.
- Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience. 2016;17(10):652-666.
- O’neil W. The relation of inner experience and overt behaviour. The Australasian Journal of Psychology and Philosophy. 1949;27(1):27-45.
- Maslow AH. Motivation and Personality Third Edition. Harper Collins Publishers; 1954.
- Mount BM, Boston PH, Cohen SR. Healing connections: on moving from suffering to a sense of well-being. Journal of Pain and Symptom Management. 2007;33(4):372-388.
About the writer

Dr Johanna Lynch MBBS PhD FRACGP FASPM Grad Cert (Grief and Loss) is a retired GP who writes, researches, teaches, mentors and advocates for generalist and transdisciplinary approaches to distress that value complex whole person care and build sense of safety. She is an Immediate Past President and Advisor to the Australian Society for Psychological Medicine and is a Senior Lecturer with The University of Queensland’s General Practice Clinical Unit. She spent the last 15 years of her 25 year career as a GP caring for adults who are survivors of childhood trauma and neglect. She consults to a national pilot supporting primary care to respond to domestic violence.